I. Introduction: Illuminating the Operative Field
In the high-stakes environment of the operating room, shadows are more than just an annoyance—they are a distinct risk to patient safety. Every surgeon knows the frustration of relying solely on overhead lights, which often fail to penetrate deep, narrow cavities or wash out critical tissue details. This is where a high-quality surgical examination headlamp transitions from a simple accessory to a vital instrument for success. It isn’t just about making things brighter; it is about ensuring absolute visual certainty when seconds count.
Gone are the days of hot, yellowing halogen bulbs that fade mid-procedure. Today’s market is driven by sophisticated LED technology, yet navigating the technical specifications can be overwhelming for even the most experienced buyer. Whether you are evaluating the specific lumen luminosity required for intricate neurosurgery or seeking ergonomic beam sculpting to minimize neck strain during marathon procedures, the right equipment is essential. This guide cuts through the noise, exploring the evolution of surgical lighting and the key features that ensure precision, safety, and superior outcomes.
II. The Technological Evolution: Why LED Has Eclipsed Halogen
The transition from halogen to LED in the medical sector was not merely a trend; it was a necessary evolution driven by the need for reliability and safety. For decades, halogen systems were the standard, yet they came with significant operational drawbacks that modern surgery can no longer tolerate.
The End of the Halogen Era
Traditional halogen bulbs operate on a physics model that is inherently inefficient for the operating room (OR). They function by heating a filament until it glows, which creates two primary problems:
- Rapid Heat Buildup: Halogen lamps generate substantial infrared heat. In a long procedure, this heat radiates onto the surgeon’s forehead and, more dangerously, toward the patient’s tissue, posing a risk of desiccation (drying out) of sensitive organs.
- The “Dim-Over-Time” Failure Mode: Halogen bulbs have a relatively short lifespan—typically around 1,000 hours. However, they rarely fail instantly. Instead, they suffer from lumen depreciation, slowly becoming dimmer and more yellow as the filament degrades. This forces the surgeon’s eyes to work harder to compensate for the lack of contrast, leading to preventable fatigue.

The LED Advantage
The shift to a high-intensity LED surgical headlight represents a quantum leap in performance. Light Emitting Diodes (LEDs) are solid-state devices that offer tangible benefits:
- Longevity: A quality LED emitter is rated for 50,000+ hours of operation. To put that in perspective, a surgeon could operate for 4 hours a day, 5 days a week, for over 40 years before the LED would theoretically need replacement.
- Consistency: Unlike halogen, high-quality LEDs maintain peak brightness throughout the entire battery cycle. The light output at minute 1 is identical to the output at minute 240.
- Efficiency: LEDs consume 70–80% less power than their predecessors. This efficiency is the key enabler for the cordless medical headlamp for surgeons, allowing for lightweight batteries that last an entire shift without tethering the surgeon to a wall console.
Emerging Tech
We are also witnessing the dawn of “smart” illumination. Emerging trends include camera integration for recording procedures from the surgeon’s POV and AI-assisted adaptive beam optics that may eventually auto-adjust brightness based on the reflectivity of the tissue being viewed.
III. The Physics of Perception: Deciphering Light Quality Specifications
When reading a spec sheet, it is easy to get lost in the numbers. However, three metrics dictate whether a light will help you distinguish a nerve from a vessel or whether it will simply blind you with glare.
Lux vs. Lumens: Understanding Intensity in Deep Cavities
Manufacturers often market “Lumens,” which is the total amount of light emitted in all directions. For a surgeon, this is largely irrelevant. The metric that matters is Lux—the amount of light that actually arrives at the surgical site.
- Surface vs. Deep Cavity: A dermatologist examining a mole might only need 30,000 lux. However, surgical lighting solutions for deep cavity procedures, such as spinal fusions or transoral robotic surgery, require significantly more power to overcome the inverse square law of light dissipation.
- The Standard: Look for a portable surgical examination light that delivers between 40,000 to 160,000+ lux. High-end units designed for neurosurgery may push even higher, ensuring that the bottom of a narrow surgical corridor is as illuminated as the surface.
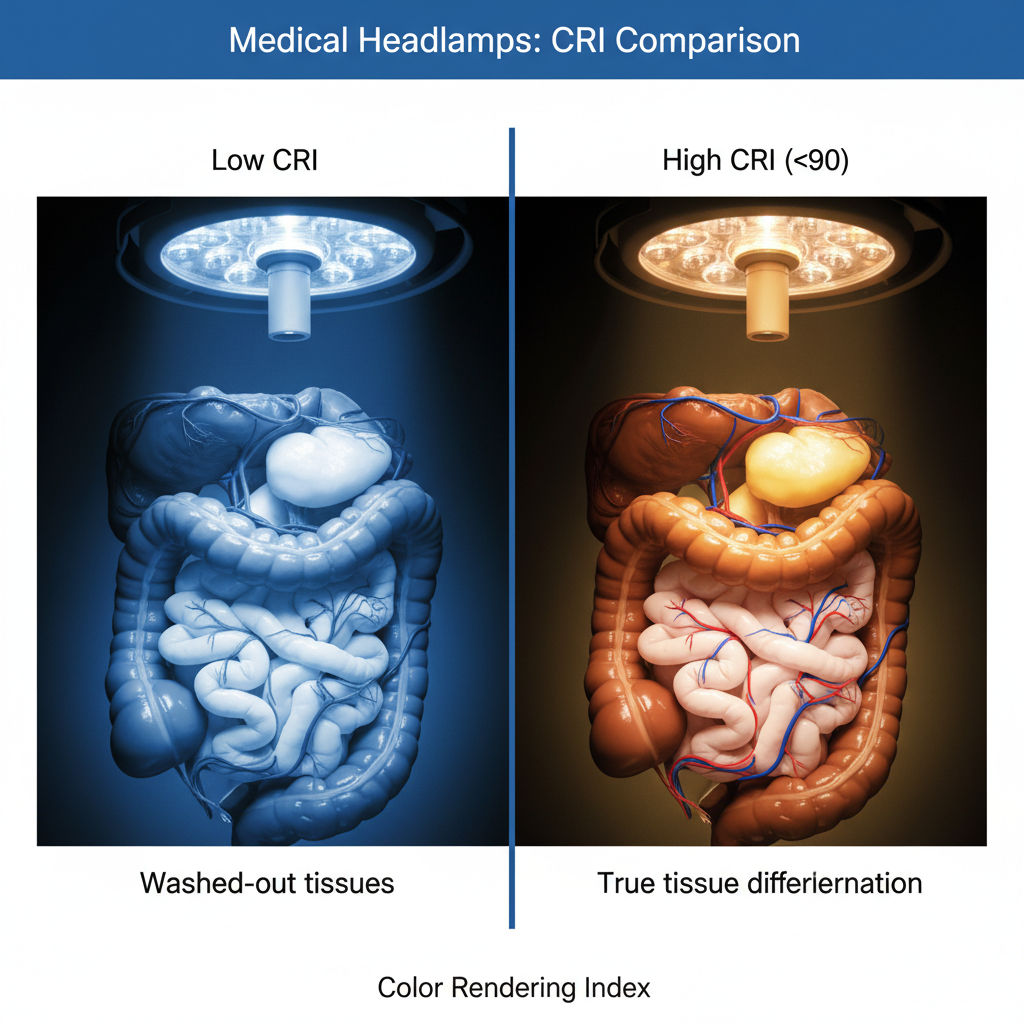
The Color Rendering Index (CRI): Why Tissue Differentiation Depends on It
Perhaps the most critical, yet overlooked, specification is the CRI. This measures a light source’s ability to reveal the faithful colors of an object compared to natural sunlight (which is CRI 100).
In the OR, differentiation is everything. A 90+ CRI rating is widely considered non-negotiable for high-stakes surgery.
- The “Washed Out” Risk: Lower quality LEDs (CRI < 80) often have a “spectral gap” in the red wavelengths. This makes oxygenated blood, muscle, and nerves all appear as varying shades of muddy brown or grey.
- Visual Precision: A CRI of 90-95+ ensures tissue color accuracy, allowing the surgeon to instantly recognize the difference between healthy vascularized tissue and necrotic tissue.

Color Temperature (Kelvin): Finding the Sweet Spot
Color temperature describes the “warmth” or “coolness” of the light.
- Warm (3000K): Too yellow (like halogen), which can distort tissue color.
- Cool/Blue (6500K+): While often perceived as “brighter,” excessive blue light causes harsh glare and rapid eye fatigue.
- The Ideal Range: Most medical studies suggest that 6100K daylight illumination or a range between 4500K – 6100K is ideal. This mimics pure solar daylight, providing a neutral backdrop that reduces cerebral processing time for visual recognition.
IV. Unbound Precision: Mobility and Battery Technology
The modern OR is crowded. Booms, monitors, anesthesia carts, and nursing staff fill the space. In this environment, a tethered fiber-optic cable is a tripping hazard and a restriction on the surgeon’s workflow.
Cutting the Cord
Professional surgical headlamp systems have largely moved to wireless designs. The benefits of a cordless medical headlamp for surgeons extend beyond convenience; they allow for 360-degree mobility around the patient table without the risk of desterilizing the back of the gown against a cable.
Battery Chemistry and Lifespan
The industry standard has shifted to the lithium-ion battery pack. These batteries are lightweight, charge rapidly, and do not suffer from the “memory effect” of older nickel-cadmium batteries.
- Runtime: A standard wireless headlamp should offer a wireless headlamp runtime duration of at least 3-4 hours on high intensity.
- Hot-Swappable Systems: For procedures exceeding typical battery life (e.g., an 8+ hour cardiac case), hot-swappable battery systems are essential. These allow the circulating nurse or surgeon to swap a depleted battery for a fresh one without the light ever turning off. This capability effectively provides an infinite runtime, ensuring operational continuity regardless of procedure length.

Placement Matters
Buyers must choose between two form factors:
- Head-Mounted: The battery is built into the headband. This is true “wire-free” mobility but adds weight to the head.
- Belt-Clip: The battery is worn on the waist, connected by a thin wire under the gown. This reduces head weight significantly but reintroduces a wire.
V. Surgeon Endurance: Ergonomics, Weight, and Heat Management
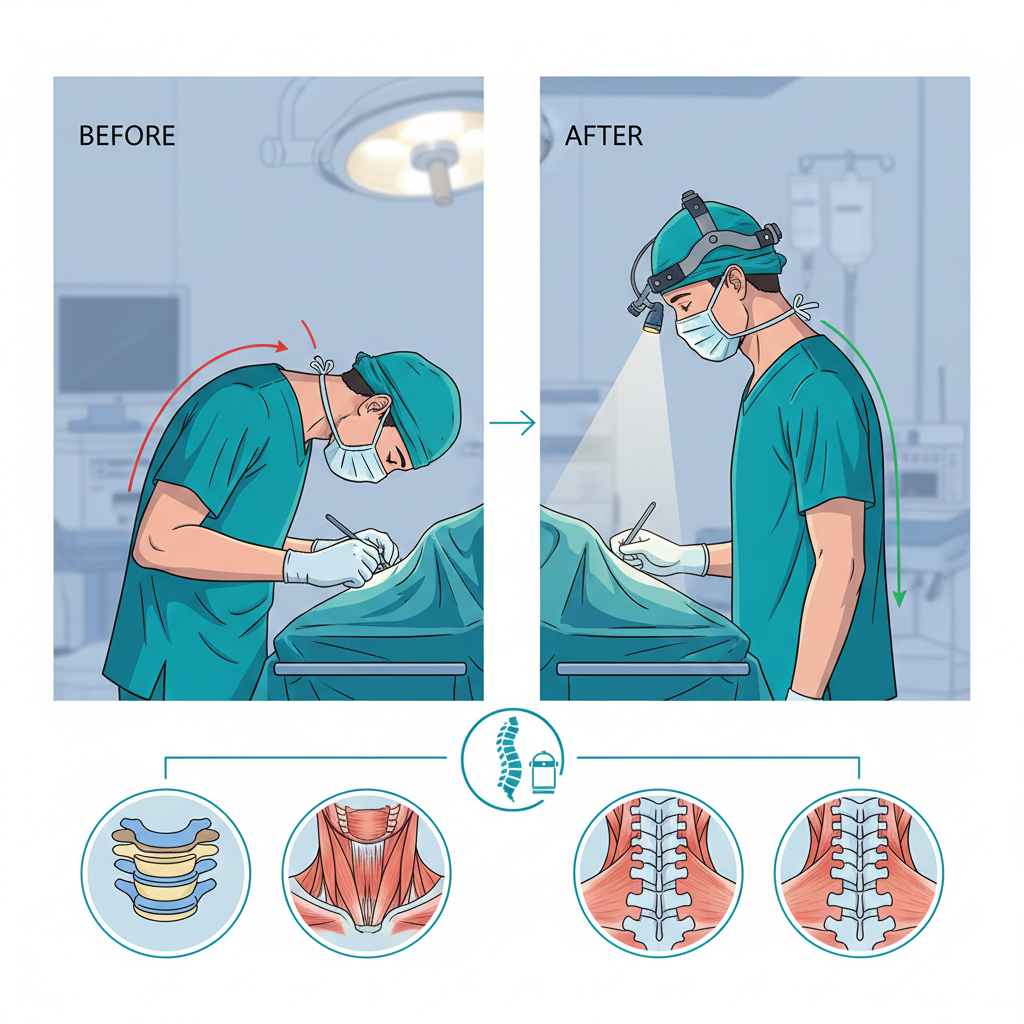
Surgical ergonomics is a career-preservation strategy. A heavy or poorly balanced headlamp can lead to chronic cervical strain, tension headaches, and early retirement.
The “Neck Pain” Factor
The average human head weighs 10-11 pounds. Adding a heavy anterior load creates a lever arm that forces the neck muscles to work overtime.
- Weight Guidelines: Look for luminaires (the light housing itself) that weigh under 6-7 oz.
- Balance: Total weight is less important than weight distribution balance. A medical grade headband light with a battery pack on the occiput (back of the head) counterbalances the front light module, keeping the center of gravity neutral over the cervical spine.
Coaxial Alignment
To achieve true shadow reduction, the light must be coaxial—meaning the beam originates from a point as close to between the surgeon’s eyes as possible. This ensures that wherever the surgeon looks, the light follows, eliminating shadows cast by the surgeon’s own hands or instruments.
Thermal Management
Even efficient LEDs produce heat. High-quality units utilize an aluminum heat sink rather than plastic. Aluminum is highly conductive, pulling heat away from the LED and the surgeon’s forehead.
- Active vs. Passive: Some units use tiny, silent fans (active cooling), while others rely on engineered metal fins (passive cooling). The goal is zero-heat emission onto the skin. A hot forehead induces sweating, which can drip into the sterile field or the surgeon’s eyes.
VI. Adaptability in Action: Features That Match the Procedure
A general surgeon performing an appendectomy has different lighting needs than a plastic surgeon performing a microvascular flap reconstruction. A “one-size-fits-all” beam is rarely sufficient.
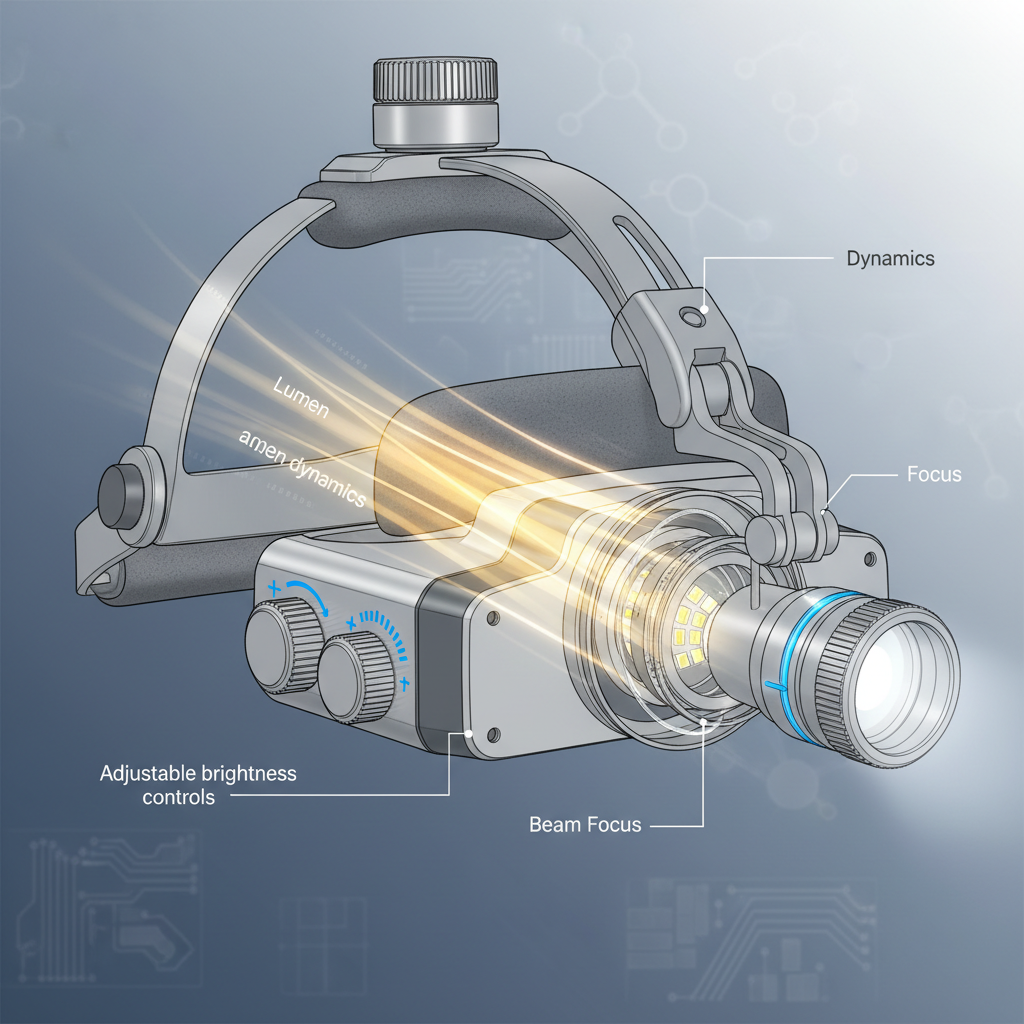
Variable Spot Size (Iris Adjustment)
Top-tier headlamps feature an adjustable spot size (often controlled by an iris mechanism).
- Range: A versatile unit should adjust from roughly 20mm to 110mm.
- Application: A wide beam (100mm+) provides context for the operative field, while a tight, focused spot (20mm) provides the intense, concentrated microsurgery lighting required for deep dissection without illuminating peripheral tissues that could cause glare.
Intensity Control
Variable intensity control is mandatory. A light that is too bright can cause “bleaching” or reflective glare on wet tissues, blinding the surgeon. Granular control allows the surgeon to dial down the light for surface work and ramp it up for deep cavities.

Customizable Fit
The headband is the interface between the machine and the human. Look for a flexible ratchet headband with dual-top straps. The “AirPad” technology found in some premium brands uses specialized foam to wick moisture and reduce pressure points.
VII. The Strategic Buyer: Calculating Value Beyond the Sticker Price
When presenting a purchase request to a hospital administration or buying for a private practice, one must look at the Total Cost of Ownership (TCO).
Upfront vs. Operational Cost
- Halogen/Fiber Optic: Lower upfront cost for the light source, but high operational costs. Fiber optic cables are fragile; the glass fibers break over time (seen as black dots in the beam), requiring frequent fiber optic replacement (costing 300−500 each). Bulbs also require frequent changing.
- LED: Higher initial investment (2,000−4,000+ for premium systems), but the operational cost is near zero. No bulbs to buy, no cables to break, and electricity usage is negligible.
- ROI: An investment analysis usually shows that a wireless LED system pays for itself within 18-24 months compared to the maintenance costs of a legacy fiber optic system.

Durability Standards
The OR is a rough environment. Equipment gets dropped, bumped, and splashed. Look for aluminum alloys and robust cabling protection. A solid warranty (3-5 years) from a reputable manufacturer (e.g., Enova, Welch Allyn, Heine, Ronin) is an indicator of build quality.
VIII. Infection Control and Sterilization Protocols
In the post-COVID era, hygiene is paramount. A headlamp that cannot be effectively cleaned is a liability.
The “Cleanable” Standard
Most headlamp units contain batteries and electronics, meaning they cannot be thrown into an autoclave. Therefore, the materials must be resistant to aggressive hospital-grade disinfectant wipes (like CaviWipes or Sani-Cloth) without cracking or yellowing.
Sterilizable Touch Points
During surgery, the surgeon is sterile, but the headlamp (worn on the head) is not. If the surgeon needs to adjust the light angle, they cannot touch the lamp.
- The Solution: Look for a sterilizable positioning handle or joystick. This is a detachable component that can be autoclaved. The circulating nurse clips it onto the lamp, allowing the sterile surgeon to adjust the beam direction safely. Alternatively, many systems utilize sterile disposable sheaths.

IX. Regulatory Compliance and Safety Standards
Purchasing non-compliant equipment opens the facility to significant legal and safety risks.
FDA Classification
In the United States, surgical headlamps are regulated by the FDA.
- FDA Class I vs. Class II: Simple lights may be Class I (General Controls), but specialized surgical lights often fall under FDA Class II device regulations, requiring 510(k) clearance to prove they are safe and effective.
- Why it matters: 510(k) clearance ensures the device has been rigorously tested for heat dissipation and electrical safety.
International Standards
- CE Marking: For the European market, the CE mark confirms compliance with the Medical Device Regulation (MDR).
- IEC 60601: This is the global benchmark for medical electrical equipment safety. It tests for risks like electrical shock and electromagnetic interference (ensuring your light doesn’t mess with the anesthesia monitor).
- Blue Light Hazard: High-intensity LEDs can emit blue light levels that are damaging to the retina over time. Compliant medical lights are tested to ensure spectral composition is safe for long-term exposure.
X. Common Pitfalls: Where Buyers Often Go Wrong
Even smart buyers can make mistakes by focusing on the wrong metrics.
- The “Brightness Trap”: Thinking “brighter is always better.” A 200,000 lux light is useless if it creates so much glare that you can’t see the texture of the tissue. Anti-glare optics are just as important as raw power.
- Ignoring Color Rendering: Buying a cheaper light with a CRI of 75. This saves money upfront but may lead to increased operative time or diagnostic errors because the surgeon cannot clearly distinguish anatomical structures.
- Overlooking Comfort: Purchasing a unit based on specs alone without trialing the fit. A light that causes a headache after 45 minutes will eventually be abandoned by the surgeon, resulting in wasted capital.
- The “Generic” Mistake: Buying non-medical grade headlamps (e.g., high-end camping or dental loupe lights not rated for surgery). These often lack the deep cavity visibility focus and the hygiene standards required for the OR.
XI. Conclusion: Investing in Visual Certainty
When you strip away the marketing jargon, the value of a surgical examination headlamp comes down to three non-negotiable pillars: High CRI/Clarity, Ergonomic Comfort, and Reliable Power.
A light that is bright but heavy will shorten the surgeon’s career. A light that is comfortable but casts shadows will lengthen the patient’s procedure. The “Holy Trinity” is finding the balance where the technology disappears, and the surgeon is left with nothing but pure, shadow-free, natural illumination.
Final Recommendation: Specifications on paper are a good starting point, but they are no substitute for clinical experience. We strongly advise buyers to arrange “try-before-you-buy” trials. Put the high-intensity LED surgical headlight on your surgeons’ heads during actual cases. Let them feel the weight distribution, test the hot-swappable battery systems, and verify the tissue color accuracy with their own eyes. Only then can you be confident that you are investing in a tool that truly enhances the safety and precision of the operative field.