True surgical precision begins with absolute visibility, yet even the most advanced operating rooms often struggle with the limitations of static overhead lighting. Shadows and fixed angles can inadvertently obscure critical details, making personal surgical lighting solutions not just a luxury, but a necessity for patient safety. This is where modern medical examination headlamps shine, offering the focused illumination in clinical settings that traditional fixtures simply cannot match.
Whether you are a specialist requiring high lumen density for deep cavity work or a procurement officer weighing complex buyer decision factors, this guide is your roadmap. We move beyond basic brightness to explore how chromatic fidelity and a high Color Rendering Index (CRI) ensure accurate tissue differentiation when it matters most. From lightweight, portable headlamps for exams to robust power management systems, we will help you navigate the technical landscape to find the perfect optical fit. Let’s illuminate the details that truly drive clinical excellence.

The Evolution of Surgical Lighting: Halogen vs. Xenon vs. LED
To understand the current state of the market, one must appreciate the trajectory of surgical illumination. For decades, the operating theater was dominated by Halogen and Xenon fiber-optic systems. While these “legacy systems” provided high intensity, they came with significant operational baggage.
Halogen bulbs, while cost-effective initially, suffered from rapid degradation of light quality—often shifting yellow as the filament aged—and generated substantial heat. Xenon improved upon brightness and color temperature but introduced a new set of problems: high replacement costs, fragile ceramic bulbs, and light boxes that acted as massive heat generators in an already warm OR. Furthermore, both systems required the surgeon to be physically tethered to a light source via heavy fiber-optic cables, restricting movement and contributing to cervical strain.
The LED Revolution
The shift toward LED surgical headlights represents a paradigm shift in medical lighting technology. Light Emitting Diodes (LED) have effectively democratized high-quality illumination by solving the “heat vs. brightness” equation.
- Solid-State Durability: Unlike fragile filaments, LEDs are solid-state devices. They are impervious to the vibrations and minor impacts common in mobile clinical environments.
- Thermal Management: Modern LEDs convert a higher percentage of energy into light rather than waste heat. This “cool” light emission is critical for preventing tissue desiccation (drying out) during prolonged open surgeries and reducing surgeon perspiration.
- Longevity: With an LED bulb lifespan often exceeding 50,000 hours, the logistical headache of maintaining an inventory of spare bulbs is virtually eliminated.

Decoding the Spectrum: Key Optical Specifications
When reviewing a spec sheet, it is easy to be dazzled by high numbers. However, for a clinical buyer or a practicing surgeon, raw power is useless without control. Here is how to interpret the data that matters.
Illumination Intensity: The Lux Myth
Illumination intensity is measured in Lux. While it is tempting to assume “brighter is better,” excessive brightness can cause glare and retinal fatigue.
- General Exams: 30,000 to 50,000 Lux is typically sufficient for dermatology, family practice, or superficial evaluations.
- Surgical Contexts: Deep cavity work (abdominal, thoracic, neuro) demands 100,000 to 200,000 Lux to punch through the darkness of a narrow surgical corridor.
Critical Insight: Look for depth of illumination. A cheap light is bright at the surface but fades inches deeper. High-quality optics maintain intensity throughout the depth of the incision.
Color Rendering Index (CRI) and Tissue Differentiation
Perhaps the most overlooked metric in clinical lighting solutions is the Color Rendering Index (CRI). Measured on a scale of 0–100, CRI indicates how accurately a light source reveals the true colors of an object compared to natural sunlight.
In surgery, this is non-negotiable. You are not lighting a warehouse; you are distinguishing between an artery, a vein, and a nerve.
- CRI < 85: Colors appear washed out or grayish.
- CRI > 90: Essential for accurate tissue differentiation. It allows the surgeon to see subtle changes in vascularity, identify healthy vs. necrotic tissue, and recognize pathology instantly.
Color Temperature (Kelvin)
The color temperature in surgical lighting dictates the “warmth” or “coolness” of the white light.
- The Sweet Spot (4500K – 5500K): This range provides a neutral white light that mimics mid-day sunlight.
- The Danger Zones: Going too “cool” (6000K+) introduces a blue tint that can distort red tissue perception and increase eye strain over varying shifts. Going too “warm” (3000K) creates a yellow cast that masks inflammation.
Shadow Control Technologies
Even the brightest light is useless if your instruments cast pitch-black shadows. Premium headlamps utilize coaxial alignment, where the light beam originates from a point directly between the surgeon’s eyes (or as close as possible), ensuring that whatever the surgeon looks at is illuminated, regardless of angle.
Tethered vs. Wireless: Choosing Your Mobility Profile
The choice between a tethered system and a cordless surgical headlight is often a trade-off between raw power and absolute freedom.
Cordless Surgical Headlights: The Modern Standard
For the vast majority of procedures, wireless is the future. The elimination of the fiber-optic cable removes a significant trip hazard from the OR floor and allows the surgeon to move freely between the operating table, imaging screens, and the sterile field.
- Ideal For: Plastic surgery, ENT, dentistry, and general surgery.
- Example: Technologies found in models like the KD-205AY-2 offer this freedom, integrating sufficient power directly into the headset without the burden of a cable.
Tethered (Fiber Optic/Cable) Systems
Despite the wireless trend, tethered systems remain relevant for extremely long, high-intensity cases. By moving the batteries and light engine to a belt pack or a separate console, the head weight is drastically reduced, and the light output can be driven higher without overheating the headset.
- Ideal For: 10+ hour neurosurgical cases or organ transplants where maximum Lux is required continuously.
Hybrid Solutions
Many modern systems now offer hybrid capability—operating wirelessly for mobility but allowing a “plug-in” to a belt pack for extended runtime, offering the best of both worlds.
Ergonomics and Comfort: The Surgeon’s Perspective
A headlamp that causes a tension headache an hour into a six-hour procedure is a liability. Ergonomic design is not just about comfort; it is about preventing long-term cervical injury.
Weight Distribution Mechanics
The total weight of the unit is secondary to where that weight sits.
- Cranial Support: Look for “Cross-Cranial” or double-strap designs (a crown strap and a circumference strap). This distributes the weight over the top of the skull rather than relying on clamping force around the forehead, which restricts blood flow and causes headaches.
- Counterbalancing: Battery placement at the back of the head helps counterbalance the optic module at the front, neutralizing the “toppling forward” sensation that strains the neck muscles.
Headband Architecture
Rigid plastic bands are durable but can create pressure points. Premium medical examination headlamps utilize flexible materials with moisture-wicking comfort padding systems. These pads should be removable and washable for hygiene.
Heat Management
In a wireless surgical headlight, the battery and LED are on your head. Efficient heat sinks are vital to ensure the lamp head remains cool to the touch. No surgeon wants a heat source radiating against their forehead while focused on a delicate anastomosis.
Power Management: Battery Life and Efficiency
Reliability is the currency of the operating room. A light that fails mid-procedure is unacceptable.
Runtime and Hot-Swapping
Battery life for headlamps must be evaluated against your typical case load.
- Standard Runtime: 3 to 5 hours is typical for high-intensity settings.
- The Hot-Swappable Standard: For continuous operation, hot-swappable batteries are non-negotiable. This feature allows the circulating nurse to swap a depleted battery for a fresh one without the light flickering or the surgeon taking the unit off.
- Rechargeable Options: Modern Lithium-Ion cells have no memory effect. Systems that utilize standardized rechargeable cells, such as those discussed regarding the KD-205AY-1 , allow for rapid turnaround between cases.
Fuel Gauges
An often-overlooked feature is the charge indicator. A visible “fuel gauge” on the headset or battery pack allows the team to anticipate power needs rather than reacting to a low-battery warning light.

Specialty-Specific Considerations
One size does not fit all. Different clinical specialties have unique visual requirements.
Neuro & Spine: The Deep Cavity Challenge
These surgeons work in deep, narrow channels. They require:
- Maximum Lux: 100k+ is standard.
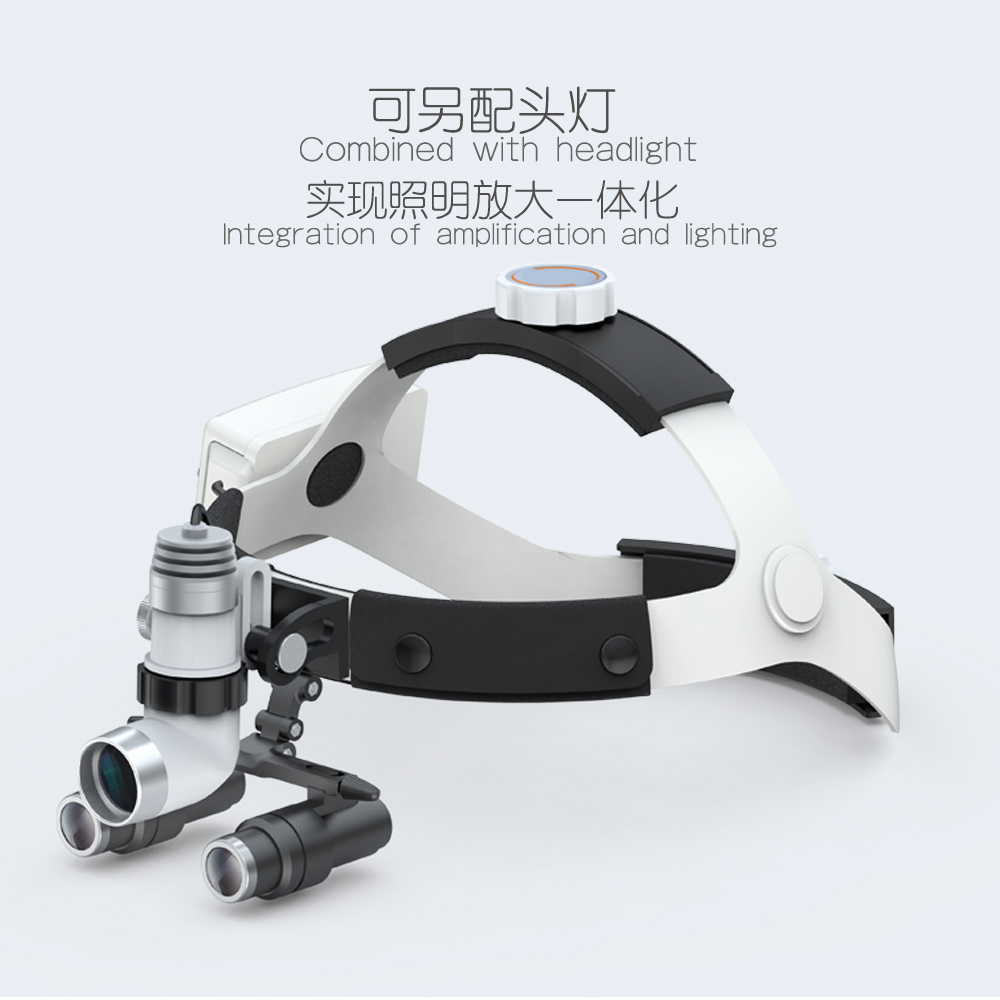
- Loupes Compatibility: The light must mount seamlessly over surgical loupes without obstructing the visual axis.
- High-Intensity Solutions: Devices engineered for these rigors, similar to the KD-203AY-7 , focus on delivering high-intensity beams that penetrate deep into the surgical cavity without diffusion.
Dentistry & Oral Surgery
The oral cavity absorbs light.
- Shadow-Free Illumination: Crucial due to the blockage caused by hands and instruments in a small space.
- Yellow Filter: A curing filter is essential to prevent the premature hardening of UV-sensitive composites during restorative work.
ENT & Otolaryngology
- Spot Size Precision: ENT surgeons need a very tight, adjustable spot size to illuminate the ear canal or nasal passage without blinding reflection from the speculum.
General Examination & Veterinary
For veterinary surgical lighting or general clinic exams:
- Portability: Lightweight is key.
- Durability: Animal patients can be unpredictable; the equipment must be robust.
Smart Features and Modern Innovations
The digitization of the OR has reached the headlamp.
Adjustable Spot Diameter
The ability to change the light field diameter is critical. An adjustable beam angle allows the surgeon to flood the area for initial exposure and then constrict the iris for a focused spotlight on the pathology. This is typically achieved via a mechanical iris aperture or electronic focusing.
Integrated Video Systems
Integrated camera headlamps are transforming medical education and documentation. These units capture the surgeon’s exact point of view (POV), allowing for:
- Live streaming for teaching residents.
- Video documentation for patient records.
- Telemedicine consultations in real-time.
Touchless Control Systems
Infection control is paramount. New touchless control systems utilize motion sensors, allowing the surgeon to adjust illumination intensity with a wave of a hand, eliminating the need to break sterility to touch a dial or ask a nurse to adjust the light.
The Clinical Buyer’s Guide: Procurement Strategy
For the procurement officer or practice manager, the decision extends beyond optics to economics and risk management.
Assessing ROI
Price is what you pay; value is what you get.
- Upfront vs. Lifecycle Cost: A cheap halogen unit is inexpensive to buy but costly to run (bulb replacements, fiber optic cable breakage). An LED surgical headlight has a higher initial capital cost but virtually zero maintenance cost over 5 years.
- Efficiency Gains: Better lighting leads to faster procedures and fewer errors.
Regulatory Compliance
Ensure the device is a recognized FDA-approved medical device (or CE marked for Europe). This guarantees the device meets electrical safety standards (IEC 60601-1) and photobiological safety standards (preventing retinal damage from blue light hazard).
Vendor Support & Warranty
- Loaner Programs: If a unit needs service, does the vendor provide a loaner? Downtime means cancelled surgeries.
- Warranty Specifics: Distinguish between the warranty on the “light engine” (often 3-5 years) and the “consumables” like batteries and cables (often 1 year).
Maintenance, Sterilization, and Care
Protecting your investment ensures consistent clinical performance.
Infection Control Protocols
- Surface Cleaning: Most portable surgical lights are not autoclavable. They are designed for “wipe-down” disinfection using standard quaternary ammonium or alcohol-based hospital cleaners.
- Sterile Handles: For lights with manual focus handles, ensure the vendor provides autoclavable snap-on covers or sterile handles so the surgeon can adjust focus mid-case.
Battery Health
Lithium-ion batteries prefer to be kept charged.
- Storage: Do not store batteries fully depleted for long periods.
- Cycling: Rotate your battery stock so all units get equal usage.
Preventative Maintenance
- Cable Care: For tethered systems, fiber optic cables are glass. Never tightly coil them; use a wide loop to prevent fracturing the fibers (which results in dimming).
- Hinge Checks: Regularly tighten the hinge mechanisms on the headset to prevent the light from “drifting” downward during procedures.
FAQ: Common Questions from Clinical Buyers
Q: Can I use a dental headlamp for general surgery?A: It depends on the intensity. Many high-end dental lights offer 50k-80k Lux, which is sufficient for minor general surgery. However, for deep cavity work, a dedicated surgical headlamp with 100k+ Lux and a larger battery capacity is recommended.
Q: How often do rechargeable batteries need replacement?A: Lithium-ion batteries typically retain optimal capacity for 300–500 charge cycles. In a busy hospital, this translates to replacing battery packs roughly every 18–24 months to ensure full runtime.
Q: What is the difference between Lux and Lumens in a medical context?A: Lumens measure the total light coming out of the bulb. Lux measures the light that actually hits the surface (the patient). For surgeons, Lux at the working distance (e.g., 40cm) is the only metric that matters.
Q: Are wireless headlamps heavy?A: Not anymore. Modern lightweight surgical headlamps use high-density battery cells and composite materials. Many weigh less than 350g (12oz), and with proper counterbalancing, they feel even lighter.
Conclusion: Lighting the Way Forward
The selection of a medical headlight is a decision that reverberates through every procedure. It affects the surgeon’s fatigue levels, the speed of the operation, and ultimately, the safety of the patient.
When choosing between the myriad of surgical lighting solutions, remember the “Golden Trinity”: Comfort, Brightness, and Battery Life. Do not be swayed by raw brightness specifications alone. Prioritize a high Color Rendering Index for tissue differentiation, a beam quality that eliminates shadows, and an ergonomic design that disappears when you put it on.
Whether you are upgrading a single private practice or outfitting a Level 1 Trauma Center, the goal remains the same: to see clearly, so you can heal effectively. We encourage you to request demos and experience the difference that precision illumination makes in your hands.


